Living safely and independently
Many people live alone. Living in a place that is safe, familiar and comfortable can help you live well with dementia. Having dementia presents challenges for your safety, but there are things you can do to manage the risks.

The COVID-19 pandemic has made it more challenging to live alone with dementia. Get some tips on managing through COVID-19 and download our tip sheet (PDF).
What to consider when deciding whether you should continue living alone
"Accept no one’s preconceived definition of who you are living with dementia. Define yourself and what makes you who you are, [including] your hobbies, your interests and your relationships. I tend not to think about the challenges or how things will look down the road, and instead, focus on day-to-day life." - Roger (pictured), from Medicine Hat, Alberta. Roger lives with Alzheimer's disease. This quotation is from his interview with Dementia Connections, re-used here with their permission.
Loss of independence
You may be able to tell when living alone is no longer safe or desirable. However, it's natural that you will want to stay in your own home for as long as possible, even if there are some safety concerns.
At home, you are free to follow life-long routines, are surrounded by a familiar neighbourhood and may have a reliable circle of support. A move away from home could mean a loss of self-reliance and control in your daily life.
Premature move from home
You may feel pressured into moving out of the home earlier than necessary. Moving before it is needed may increase feelings of loneliness, and it may result in a faster cognitive decline.
Social engagement
"Develop a support system that you can rely on. You will be able to share your feelings and count on others who can help you." - Tanis (pictured), from Winnipeg, Manitoba. Tanis lives with vascular dementia.
Evidence shows that staying socially active may help slow down the progression of dementia, allowing people with dementia to live independently for a longer period of time.
Many communities offer adult day programs with transportation. These programs provide supervised activities, usually in a group setting, that promote independence, provide stimulation and encourage social interaction.
Living environments that provide safety, quality of life and support
Overall, it's important that you live in a place that best supports your safety and quality of life. For some, this may mean living at home with support services, even if there is some risk.
The amount and type of support available are important factors in determining your ability to live well alone. For example, a person with a large family living in a community with many services may be better able to live alone than someone with no family living in a community with limited services.
Use these questions to help guide your decision
"If you have dementia, you need to discover and know your limitations so you too can live well. Let people know that you are still a person, and they should talk to you about any decisions that involve you – don’t be afraid to ask for help." - Sandra, from Halifax, Nova Scotia. Sandra lives with dementia with Lewy bodies with Parkinson's.
In page three of our brochure, Conversations about dementia and living alone, there is a questionnaire that asks a person to assess whether they can continue living alone. By getting someone you trust to fill out this questionnaire, you can get more insight on where you stand. However, be prepared to read an assessment that you may not agree with.
The information on this page is also available to read in a print-friendly PDF. Download Conversations about dementia and living alone or contact your Society for a copy.

Strategies to help you stay safe
Here are some strategies that can help reduce risks and ensure your safety.
Leave a set of house keys with trusted neighbours
- Access to the home is available.
- Someone can enter the home if help is needed.
- If one neighbour is not always at home, consider leaving a set of keys with two different neighbours.
Arrange for someone you trust to call or visit once a day
- Regular check-ins can reassure you well as your family and friends.
- Timing can help ensure that you eat or take medication.
- This person may be able to monitor areas of concern you have.
- If problems arise between calls or visits, consider checking in with the person twice a day. This can be a quick phone call in the morning and a second phone call late afternoon.
Appliance safety measures to minimize the chance of an accident
- Get an automatic shut off kettle.
- If you're concerned about stove safety, you can remove fuses, remove knobs, put burners on timers and shut off the gas. Consider using a toaster oven or a microwave for heating food instead – they are good alternatives and allow use of pre-prepared foods with little work.
- Lower the temperature of the hot water heater.
Post a visible, easy-to-read list of emergency phone numbers
- Consider adding a picture beside the name and telephone number.
- Consider adding speed dial numbers (if phone has this feature) with pictures.
- Consider getting a phone with a limited number of features (e.g., preprogrammed phone numbers).
- This list may not always be handy in certain situations. For example, you may have a fall away from your phone. Consider purchasing an alert button that allows you to call for help in an emergency situation, or a fall detection device.
Adapt your home to prevent falls
Falls are the leading cause of injury-related deaths for older adults, and people who live with dementia are especially at risk of falling. The following strategies may help you modify your home in order to reduce the risk of falls:
- Ensure that there is good lighting. Make sure that each room has enough light, and reduce dark areas and shadows.
- Clear walking paths inside the home by removing tripping hazards such as a loose rug or electrical cords.
- Reduce clutter inside and outside the home. Ensure that there are no dips in walkways outside the home or uneven ground.
- Purchase safe footwear. Shoes that have velcro fastenings are a good option as they are easy to take on and off.
- Place night lights throughout the home for when you need to go to the bathroom or kitchen during the night.
- Install railings inside and outside the house and grab bars in the bathroom for extra support.
- Use non-slippery bath mats and place non-slip strips in the bath/shower. Avoid using a dark colour bath mat, as it could be mistaken for a hole. Buy a mat that matches the colour of the bath/shower.
- Remove soap build-up in the tub or shower on a regular basis to avoid slipping.
Visit Finding Your Way®
Finding Your Way® is a website dedicated to helping you balance the risks of living with dementia while enjoying a healthy and safe lifestyle.
Through Finding Your Way®, you can get strategies for living an active, safe and engaging lifestyle. You can also learn how to prepare for risks to your safety that become more likely as your dementia progresses, such as the chance of getting lost.
Note that while the Finding Your Way® service is only available for people living in Ontario, the website has information and resources can help you live safely in your community, no matter where you live in Canada.
Consider arranging for an Occupational Therapist to come into the home for a safety assessment. Visit https://www.caot.ca/site/findot to find an occupational therapist near you.
Strategies to help you take charge of your health
Living with dementia brings many life changes. When we are caught up in our daily lives, we don’t always look after ourselves. It's important to look after your general health as you face the challenges of dementia. Consider these strategies to ensure that you're as healthy as you can be.
Schedule and maintain your appointments
- See your doctor regularly for checkups and to address specific health concerns.
- Numbers count – keep your blood pressure, cholesterol, weight and blood sugar within recommended ranges.
- Have regular vision and hearing tests. Being unable to see or hear properly can contribute to stress and confusion.
- Visit a dentist regularly.
Get adequate sleep
Sleep deprivation can significantly impair your memory, mood and function.
Consider meal programs and services
- Food delivery programs like Meals on Wheels can provide you with a nutritious, hot meal once a day and provide fresh fruit and vegetable baskets.
- Other community support programs, such as community dining, can give you an opportunity to socialize.
- Grocery delivery services, whether they are scheduled online or by telephone, can deliver . However, know that these services can be costly.
Use prepared foods, nonperishable foods and foods that do not need to be stored in a refrigerator
Preparation is easier, and you will likely be less concerned about spoilage.
Simplify your medication routines
- Use a pill dispenser.
- Have someone visit to drop off your pills.
- Consider a blister pack prepared by a pharmacist. This can have the added benefit of building a relationship with your local pharmacy.
Strategies to help your memory
Memory loss can be difficult to cope with and frustrating. However, there are strategies that you can use to help you manage your memory problems and stay independent for as long as possible.
Fill out the All about me booklet
- As your dementia progresses and it becomes more difficult to manage the changes in your abilities, it's important that you record the things that make you the person you are.
- All about me is a booklet that can help you tell others about yourself. Through All about me, you can focus on the positive: What you are good at, rather than what is no longer possible.
- An editable PDF version of All about me is available for download, which allows you to type your information directly into the document.
Use memory aids and tools
- Post-it notes are a great way to write down reminders as needed or as you think of them.
- Dry/erasable whiteboards are another great tool to help you remember things. Whiteboards come in a number of different sizes that can be hung on a wall.
- Almost all ovens have a timer, and if yours doesn’t, you can buy one at many department or hardware stores.
Follow visual cues
Visual cues can be very helpful for remembering things. For example:
- Hanging a backpack on your door handle can serve as a reminder to take it with you when you leave your home.
- Leaving a slow cooker or a bread maker on the counter will remind you that you want to prepare a meal or make bread.
- Putting your laundry hamper in your living room will remind you that you need to do laundry.
Your imagination is the only limit on how you can use visual cues to help you remember things!
Get more tips and resources that can help you manage challenges with memory.
Strategies to help you handle your finances
The following are strategies to help you handle day-to-day financial transactions, such as paying bills promptly, and to help reduce the risk of financial exploitation or abuse.
Use bank-at-home services
- These services are available online and by telephone. Check with your bank to see how this service can be set up for you.
- This way, you don't need to leave your home to go to the bank.
- These services can be personalized to your needs.
Set up direct deposit of cheques and automatic withdrawal for bill payments
This hands-free approach to banking offers fewer chances for problems such as missed payments.
Arrange for someone you trust to help you manage your finances
- This could be a substitute decision-maker or a Power of Attorney.
- They can help you with writing cheques, paying bills and managing your accounts.
- This way, you can balance your independence while still protecting your finances.
Be aware and be careful
- Know that bank-at-home services, direct deposits and automatic withdrawals do not mean you are protected from overpayment/non payment of bills, or from scams.
- Talk about your finances as early in the disease process as you can.
- Register for “Do Not Call” solicitation lists.
- Consider making the bank manager at your local branch aware that you live with dementia.
- To learn more about financial risks and common scams, talk to a financial advisor.
Strategies to help you with your daily living
The following are strategies that can help you with your personal care, to remain physically and socially stimulated throughout the day, and put an emergency system in place in case you need help.
Set up an emergency call system
- This could be an alert button, for example.
- This way, you will have 24-hour access to help should a problem arise.
- Also consider products that alert when no motion is detected.
Get help with practical tasks
- Like someone that can help you in your home with housekeeping and meal preparation. For example, they can sort your closets and dresser drawers to make only the necessary clothes available.
- This way, you can get more tasks accomplished in a given day.
Consider agency support
- Agency support can help you manage your personal care, such as maintaining personal hygiene. Maintaining your personal care and hygiene will make good health and well-being come naturally.
- However, know that these services can be costly.
- As well, it's important that a strong relationship is established between you and the agency's care provider. If possible, arrange to have one consistent worker who you can build a working relationship with.
Sign up for a day program
- Helps you remain an active member of your community.
- Provides physical, social and mental stimulation that you may not get from other activities.
- You can meet other people living with dementia whom you can share your experiences with.
Be ready for an emergency department visit
Whether it is a planned admission or an unexpected emergency visit, the unfamiliar noises and activities of a hospital can be especially upsetting when you also have to manage your symptoms from dementia.
Preparation can improve a visit. Be Ready for an Emergency Department Visit is a series of handy checklists and forms for you to fill out with a family member, friend or caregiver. Complete these forms before a trip to the hospital is necessary, so that you can be ready to go.
The information provided on these forms will help you communicate your needs, making it possible for hospital staff to provide more personalized care that can help you better .
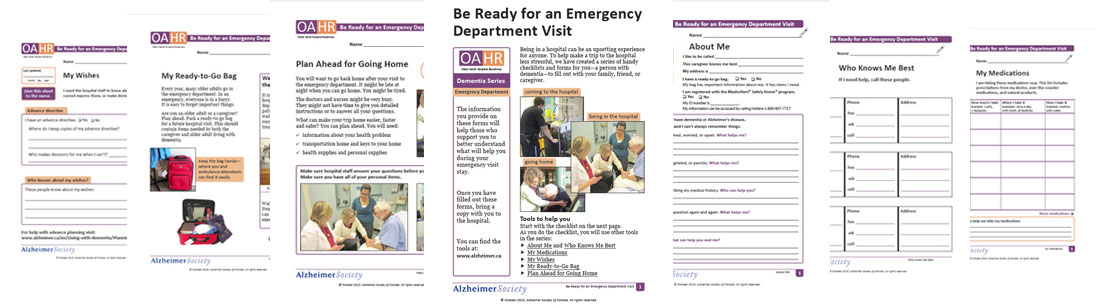
Download the checklist to get started.
Use the checklist as a guide to work through each of the tools in this series:
What to know about driving
It's important to plan ahead for the time when driving may no longer be safe for you. Look for alternative modes of transportation such as public transit, services provided by community organizations, transportation organized by family members and friends or setting up an account with a local taxi company.
To learn more about living well with dementia, you can download our Heads Up for Healthier Living brochure (print-friendly version), for people living with Alzheimer's disease and their families. Even if you have another type of dementia, the tips and strategies in this brochure can help you live well.
More useful links and resources
Conversations about dementia and living alone. Alzheimer Society of Canada, February 2018. This sheet provides information on what to consider when deciding if a person with dementia should continue living alone.
All about me. Alzheimer Society of Canada. A booklet designed for people living with dementia to help them create a record of their background and what is important to them.
Be ready for an emergency department visit - checklist. Alzheimer Society of Canada and Older Adult Hospital Readiness (OAHR), October 2015. Part of the Older Adult Hospital Readiness Dementia Series, this checklist can help people living with dementia better prepare for a visit to the emergency department. This series is the result of a research project funded by the Canadian Institutes of Health Research (CIHR) and the Alzheimer Society of Canada.
Dementia and COVID-19: Tips for people who have dementia and are living alone. Alzheimer Society of Canada, 2020. This tip sheet goes through six essential pieces of advice to help people who have dementia and are living alone manage through COVID-19.
Heads up for healthier living. Alzheimer Society of Canada, August 2014. This downloadable brochure can help people living with Alzheimer's disease and their families make lifestyle choices to stay healthy and live well with dementia. The tips and strategies in this brochure are applicable to people living with other types of dementia as well.
Memory tips & tricks. Alzheimer Society of Canada. An information sheet for strategies to help people with mild memory problems, based on ideas and suggestions provided by people living with memory loss.
Shared experiences: Suggestions for living well with Alzheimer’s disease. Alzheimer Society of Canada. This booklet, informed by the real experiences and advice of Canadians living with Alzheimer's disease, can help answer common questions and concerns about living with Alzheimer's.
Finding Your Way®: Living safely with dementia - A resource guide. Alzheimer Society of Ontario, 2017. This resource guide provides people living with dementia, caregivers and families with tips and strategies on various safety-related topics, so that people living with dementia can live safely in their day-to-day lives.
Adapting your home to living with dementia: A resource book for living at home and guide to home adaptations. Canada Mortgage and Housing Corporation, 2009. This comprehensive document can help people living with dementia, caregivers and families adapt their homes in response to the changes brought on by dementia.
Find an Occupational Therapist. Canadian Association of Occupational Therapists (CAOT). This online directory can link people living with dementia to the closest Occupational Therapist in their area.
Get ready for an emergency department visit. Older Adult Hospital Readiness (OAHR), February 3, 2016. This webinar presents a series of communication tools that can help the transition to the emergency department, the time in the emergency department and transition back home for the person living with dementia less distressing. Hosted by brainXchange in partnership with the Alzheimer Society of Canada and the Canadian Consortium of Neurodegeneration in Aging (CCNA).
